Almost everybody knows that there are potential risks with eating raw cookie dough (or any other raw batter). However, much of that risk was thought to be due to the potential of salmonella from raw eggs and so, if the plan was to eat, rather than cook, the dough, the eggs could just be left out. No more! say health experts. Turns out that just removing the eggs and eating the raw dough may protect you from salmonella, but it still leaves you at risk for E. coli.
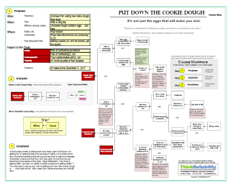
Once the impacted goals are captured, they become the first “effects” in the cause-and-effect relationships. The Cause Map is created by capturing all the causes that led to an effect. In this case, the risk of contracting salmonella from eating raw cookie dough results from eggs being exposed to salmonella, and the salmonella not being effectively destroyed (by the heat of baking). The risk of contracting E. coli results from a similar issue.
Cookie dough contains raw flour. The cooking process kills E. coli (as well as salmonella), meaning cookies and other baked goods are safe to eat, but dough is not. Distributed raw (uncooked) flour was found to be contaminated with E. coli (leading to the impacted environmental goal and the recall). The flour was likely contaminated with E. coli while it was still wheat in the field. Birds and other animals do their business just about wherever they want, and it’s got some bacteria in it, meaning that excrement that falls on wheat fields can deliver contamination to pre-flour. (Quick side note: we frequently get asked when to stop asking “why” questions. When you get to an answer that is completely outside your control, like why birds poop in wheat fields, for example, this is a good place to end the cause-and-effect reasoning.)
While flour is processed, the process isn’t designed to completely kill pathogens (unlike pasteurization, for example) and according to Martin Wiedmann, food safety professor at Cornell University, “There’s no treatment to effectively make sure there’s no bacteria in the flour.” Flour is not designed to be a ready-to-eat product.
Once the causes related to an issue have been developed, the next step is to brainstorm and select solutions. Unfortunately, health professionals have been clear that they’re not getting far on keeping birds from pooping in fields, nor is there some sort of miracle treatment that will ensure raw flour is safe from disease. (Scientists underscore that flour isn’t less safe, it’s just that we are becoming more aware of the risks. Says Wiedmann, “Our food is getting safer, but also our ability to detect problems is getting better.”) The only way to reduce your risk of getting sick from raw cookie dough is . . . not to eat it at all. Also, wash your hands whenever you handle flour. (This is of course after you’ve thrown out the floor involved in the recall, which you can find by clicking here.)
To view the Cause Map of the problems associated with raw cookie dough, please click on “Download PDF” above.




