The risk associated with medical treatment administration is high. There is a high probability for errors because of the complexity of the process involved in not only choosing a treatment, but ensuring that the amount and rate of treatment is appropriately calculated for the patient. The consequence associated with treatment errors is significant – death can and does result from inappropriately administered treatment.
Medical treatment includes delivery of both medication and radiation. Because of the high risk associated with administering both medication and radiation therapy, independent checks are frequently used to reduce risk.

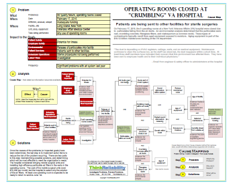
However, in a case last year in Scotland, a patient received a significant radiotherapy overdose despite the use of independent checks, and verification by computer. In order to better understand how the error occurred, we can visually diagram the cause-and-effect relationships in a Cause Map. The error in this case is an impact to the patient safety goal, as a radiotherapy overdose carries a significant possibility of serious harm. The Cause Map is built by starting at an impacted goal and asking “why” questions. All causes that result in an effect should be included on the Cause Map.
In this case, the radiotherapy overdose occurred because the patient was receiving palliative radiotherapy, the incorrect dose was entered into the treatment plan, and the incorrect dose was not caught by verification methods. Each of these causes is also an effect, and continuing to ask “Why” questions will develop more cause-and-effect relationships. The incorrect dose was entered into the treatment plan because it was calculated incorrectly (but the same) by two different radiographers working independently. Both radiographers made the same error in their manual calculations. This particular radiotherapy program involved two beams (whereas one beam is more common). The dose for each beam then must be divided by two (to ensure the overall dose is as ordered). This division was not performed, leading to a doubled calculated dose. The inquiry into the overdose found that both radiographers used an old procedure which was confusing and not recommended by the manufacturer of the software that controlled the radiotherapy delivery. While a new procedure had been implemented in February 2015, the radiographers had not been trained in the new procedure.
Once the two manual calculations are performed, the treatment plan (including the dose) was entered into the computer (by a third radiographer). If the treatment plan does not match the computer’s calculations, the computer sends an alert and registers an error. The treatment plan cannot be delivered to the patient until this error is cleared. The facility’s process at this point involves bringing in a treatment planner to attempt to match the computer and calculated doses. In this case, the treatment planner was one of the radiographers who had first (incorrectly) performed the dose calculation. The radiographers involved testified that alerts came up frequently, and that any click would remove them from the screen (so sometimes they were missed altogether).
The inquiry found that somehow the computer settings were changed to make the computer agree with the (incorrect) manual calculations, essentially performing an error override. The inquiry found that the radiographers involved in the case believed that the manually calculated dose was correct, likely because they didn’t understand how the computer calculated doses (not having had any training on its use) and held a general belief that the computer didn’t work well for calculating two beams.
As a result of this incident, the inquiry made several recommendations for the treatment plan process to avoid this type of error from recurring. Specifically, the inquiry recommended that the procedure and training for manual calculation be improved, independent verification be performed using a different method, procedures for use of the computer be improved (including required training on its use), and requiring manual calculations to be redone when not in agreement with the computer. All of these solutions will reduce the risk of the error occurring.
There is also a recommended solution that doesn’t reduce the risk of having an error, but increases the probability of it being caught quickly. This is to outfit patients receiving radiotherapy with a dosimeter so their received dose can be compared with the ordered dose. (In this case, the patient received 5 treatments; had a dosimeter been used and checked the error would likely have been noticed after only one.)
To view the Cause Map for this incident, please click on “Download PDF” above.